Retinal Detachment & Tears
What is Retinal Detachment?
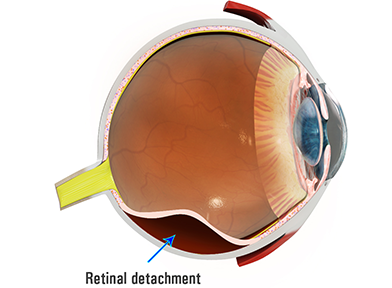
Retinal Detachment is where the thin layer of cells that lines the inside of the back of the eye (retina) develops a tear and starts losing its adhesion to the underlying eyewall tissues and blood supply.
The retina loses function when detached because nutrients cannot reach the retina.
A Retinal Detachment is a serious condition and may result in permanent loss of vision or even blindness unless treated promptly.
What are Retinal Tears?
Retinal tears are small breaks or openings in the retina. They can occur for various reasons, such as trauma, aging, or other eye conditions. If left untreated, a retinal tear can progress to a retinal detachment, where the entire retina becomes detached from the underlying layers of the eye.
Who Does Retinal Detachment Affect?
Anyone can develop a Retinal Detachment at any time. However, some people are more at risk of the condition. Predisposing factors for Retinal Detachment include:
- Age: Posterior Vitreous Detachment (PVD) occurs more commonly as we age
- Myopia - short-sightedness increases by ten times the risk of Retinal Detachment. This is because a myopic eye is larger than average and the retina is thinner and weaker and more prone to develop a tear during PVD. Myopia patients also develop PVD at a younger age,
- A family history of Retinal Detachment,
- Cataract surgery - previous intraocular surgery will slightly increase the risk,
- Trauma - previous injury to the eye or face increases the risk,
- Weak areas in the retina (Lattice Degeneration).
Patients who have developed a Retinal Detachment in one eye are also at increased risk in their other eye.
If weak areas of the retina or retinal tears are discovered in the fellow eye, preventive laser treatment may be necessary to reduce the risk to the alternate eye.
Symptoms of Retinal Detachment
Most patients observe a change in their vision.
Early symptoms of Retinal Detachment are when a patient notices:
- A dark shadow or curtain starting at the edge of the field of vision and moving centrally.
- Blurred or distorted central vision if the macula becomes detached.
- Increased sensations of flashing lights and Floaters are early symptoms caused by the vitreous gel pulling on the retina and should also be reviewed urgently.
- Flashes of light: bright and rapid flashes
These symptoms do not always mean a Retinal Detachment is present. However, you should see your ophthalmologist as soon as possible.
Sometimes, your ophthalmologist discovers a Retinal Detachment during a routine Eye Examination.
Treatment of Retinal Detachment and Tears
The treatment approach for retinal tears and detachment depends on the severity and type of the condition:
- Retinal Tears: Small retinal tears without detachment may be treated with laser therapy or cryotherapy (freezing) to seal the tear and prevent fluid from entering the subretinal space.
- Retinal Detachment Repair: Surgical intervention is usually necessary to reattach the retina and prevent vision loss. There are several surgical techniques, including:
- Pneumatic Retinopexy: A gas bubble is injected into the eye to push the detached retina back into place. Laser or freezing treatment is then applied to seal the tear.
- Scleral Buckling: A silicone band or sponge is attached to the eye's outer surface to indent the eye's wall, relieving traction on the retina. This is often combined with laser or cryotherapy.
- Vitrectomy:
In this procedure, the vitreous gel is removed from the eye, and any scar tissue or fluid causing detachment is removed. The retina is reattached using laser therapy or other methods.





